New Delhi: The Delta variant (B1.617.2), the principal cause of the second wave in India, is rapidly spreading across the world, already detected in 74 countries and poised to become the dominant strain globally.
On 14 June, scientists announced a new highly infectious Covid-19 variant in India called AY1 (B1.617.2.1), whose capacity to resist vaccines and antibody therapies is under investigation.
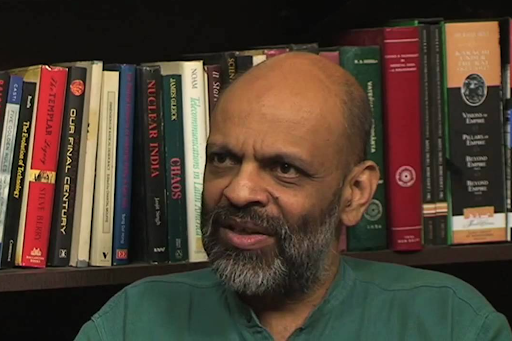
In a conversation with Article 14, eminent immunologist Satyajit Rath warned that the government’s “triumphalist hubris” without addressing several key issues, leaves the country “poorly prepared” for continuing outbreaks.
India is the only country in the world facing acute vaccine shortages despite an indigenous, public-sector developed vaccine candidate and available production capacity. It also has some of the most expensive vaccines in the world, tucked away behind a maze of apps and one-time-passwords (OTPs).
In the month of May, just nine corporate hospitals in big cities cornered 50% of the supply allocated to the private sector, according to the Indian Express. For every 1,000 men, only 867 women have got vaccinated, a proportion more skewed than India’s sex ratio of 900 (2015 figures). On 16 June 2021, 3.5% of India’s population was fully vaccinated and 15.4% had received at least one dose.
On 31 May 2021, the Supreme Court declared the Modi government’s vaccination policy for those in the 18-44 age bracket “prima facie arbitrary and irrational”, and asked the government of India to place all the official documents including file notings before itself. About 67% of Indians fall in the 18-44 age group, as per Census 2011.
On 7 June, Prime Minister Modi re-allocated the 25% quota for procurement of vaccines by state governments back to the central government. The actual share of doses going to corporate hospitals is difficult to verify, given the opacity in vaccine production and procurement.
The slow and patchy vaccination also raises problems of epidemiology and public health, according to Rath. It was entirely preventable, and the government’s failure to arrange for enough vaccines is of a piece with its broader, episodic approach that threatens to prolong the pandemic, he tells Article 14.
Trained as a physician and a pathologist, Rath has conducted research on various aspects of how immune processes work. Until retirement, he was a scientist with the National Institute of Immunology, under the department of biotechnology, and currently teaches at the Indian Institute of Science Education and Research Pune.
Edited excerpts of the interview with Rath:
How significant is the Prime Minister’s announcement of 7 June?
The union government has partially rolled back its policy asking states too to procure vaccines independently, which is welcome. At the same time, the 25% quota for private hospitals continues, which contributes to inequity.
The announcement does not address the real problem i.e. vaccine shortages. The measures it has announced for that are so recent that it will take quite some time before we see an increase in supply. Until then, there will not be any real difference on the ground.
What has been wrong with our vaccination strategy?
It is inadequate for the scale of our COVID-19 public vaccination campaign. The government did not plan for the necessary volume and pace of vaccine supply and distribution, nor for the systematic monitoring that would be crucial. The primary, critical failure of this government is the absolute refusal to acknowledge any limitation or misstep. If we had acknowledged it, then for instance, anticipating serious shortages, we would have continued vaccinating priority segments of society—health care workers, elderly people, those with relevant comorbidities—systematically. Instead, we created an extraordinary, unmanageable mess, by suddenly throwing open scarce doses to all above 18 and passing the buck to the states.
Besides the shortages, a divided supply chain and widely varying price points are leading to vaccines getting cornered by the rich and the connected. What are the implications of this in terms of public health, emergence of mutant variants, and our vaccination strategy itself?
Since last year, the world over, what we have done as a non-pharmaceutical intervention, is physical distancing. The natural selection pressure on the SARS-Cov-2 virus population therefore favors variants that circulate more efficiently. Without an exception, all the variants that have emerged, including the latest one in Vietnam, have the common property of easier transmission. This is why their spike proteins, the entry point of the infection, have changed.
And we have focussed our vaccine development strategy almost entirely on generating antibodies through the spike protein (e.g. Covishield, Pfizer, Moderna, Johnson & Johnson, Sputnik V vaccines). So as a byproduct of increasing transmission, the variants are showing some amount of loss of vaccine reactivity. This is not yet a situation where we are seeing variants selected for evading vaccines.
We have pockets of vaccinated people living cheek by jowl with large swathes of unvaccinated people. But, as we begin to vaccinate more and more people, yet less and less equitably, we will come to a point where vaccine-escape variants [i.e. variants that make vaccines less effective] will emerge. They may only be incrementally lethal, but will mean continuing outbreaks.
In August 2020, Krishna Ella, the managing director of Bharat Biotech International Ltd, had claimed that vaccines would be cheaper than bottled water. Now, Bharat Biotech has sought maximum market prices for Covaxin to recover costs of R&D and clinical trials, and funds from the government to expand its manufacturing capacity beyond 200 million doses annually. Vaccines have been sold at Rs 700-4,000 a dose. Are these prices justified?
Growing the virus, inactivating it, and using it as a vaccine is a very old technology. This is essentially how Jonas Salk developed the polio vaccine. So there is nothing particularly innovative about Covaxin. Months earlier, the Chinese government-owned Sinopharm developed an inactivated vaccine [approved in China on 31 December].
I find it hard to answer questions of 'how much profit is justified' in a capitalist system that reveres profit-making. The real question for me in this situation is, are such prices going to make vaccine accessibility difficult for people who cannot afford them? And the answer, sadly, is yes.
Covaxin relies on an inactivated SARS-Cov-2 virus isolated by the National Institute of Virology (NIV), under the Indian Council of Medical Research (ICMR). Do you think it was correct for ICMR to rely solely on Bharat Biotech for Covaxin production, given it has provided just 10% of doses administered in the country?
As NIV isolated the virus, the ICMR could have started conversations on two different fronts. First, it could have begun talks on licensing the vaccine with all the bio-generic manufacturers in the country, and asked them to gear up for production. It could have asked them to make the necessary infrastructural investments and provided some monetary support. Second, the ICMR could have pushed, in April 2020 itself, for rapid upgradation of equipment and upskilling of personnel in the public sector. By early 2021, we would then have been in a position to undertake parallel public sector manufacturing of this vaccine. However successive governments have allowed vaccine manufacturing capacity in the public sector to become utterly moribund.
Also, growing an infectious virus in large amounts demands stringent containment and safety facilities [classified as Biosafety Level (BSL)-3]. So it makes sense to decentralize production and lower and distribute the risk of industrial accidents, by processing smaller amounts of the virus in each location.
In May 2021, the union government seemed to wake up and offered grants worth Rs 220 crore to Bharat Biotech and three public sector undertakings for the infrastructure upgrade necessary to begin manufacturing Covaxin.
Yes, a year too late. Had it done this last year itself, we would have been in a comfortable situation by now. I am not sure if these sums are based on any realistic assessment of what these enterprises need for this purpose, but if so, it is all the more astonishing that the government did not consider investing even such paltry sums as 'at-risk' investments last year.
Why do you think the government did not take these steps?
Three possibilities come to mind. First, the government perhaps believes that only companies can achieve the last mile of product development, and that companies will do so only if assured of exclusive rights. This is simply not true for bio-generic manufacturers.
The second possibility is that when you have non-exclusive licenses, royalty returns are much smaller.
Finally, when the government gives non-exclusive licenses and participates in downstream product development, it needs to spend a fair amount of public funds for what I see as a public good. But as in many other instances, the government of India does not appear to be interested in spending money on the pandemic up front.
Instead, the government, and its agencies such as the DBT, DST, CSIR, ICMR, are essentially trying to convert public institutional research into revenue streams. That’s what they have done with Covaxin. Bharat Biotech may not be wrong in claiming that it did not receive much money from the government for downstream product development. All that the ICMR may have done was use government clout to armtwist and push the vaccine along as the notorious letter (setting a deadline of August 15 for vaccine development) by director general Balaram Bhargava indicated, without investing substantial government funds. This is the classic response of conservative political ideologies and Indian governments over the past 30 years.
Have other countries not managed vaccination without public-sector production?
Most vaccines in the world have come out of public laboratories and universities, but manufactured and distributed by for-profit private companies. To allow private companies to control the flow of critical vaccines as a global public good, is itself a brain dead decision—globally and in India.
Nonetheless,there certainly were steps that the Modi government could have taken. It was obvious by May 2020 that mRNA vaccines were beginning to gain traction, and by June, the Serum Institute of India (SII) had tied up with AstraZeneca. The government of India could have shared some capital investment and associated risk with SII, and in return negotiated supplies for domestic use in the contract with SII and AstraZeneca. The government could also have spoken to Moderna and Pfizer to negotiate licenses for domestic production. We could have also asked them to conduct bridging trials as they were conducting large-scale phase-3 trials, and assured them of immediate licensing and purchases if the provisional results look good. For the manufacturing licensees, the government could have promoted ancillary manufacturing for mRNA vaccines.
The failure to get even a for-profit strategy right is partly to do with the kind of backward-looking right-wing ideology favored by the political leadership of this government. The emphasis on past glories to validate the present, leads the BJP and the RSS into a triumphalist trap of never acknowledging any failure or misstep.
And, unforgivably, the Covaxin case suggests that even when the government had a vaccine in its control, it was perhaps more interested in revenue streams than saving lives.
The Brazillian health regulator is alarmed that Bharat Biotech has not taken sufficient measures to inactivate the SARS-Cov-2 virus. On 5 June, it allowed limited doses of Covaxin under strict conditions, after Bharat Biotech made certain improvements in the manufacturing process. The phase-3 clinical trial results too are delayed. What do you make of these concerns?
Regulators go by documentation. Being familiar with Indian systems, I suspect that sloppy record-keeping by Bharat Biotech is to blame here, rather than an actual problem with inactivation.
Phase-3 trials last for a year. In a phase-3 trial, you take say 40,000 people and randomly give them the vaccine or a placebo. And then every week, volunteers are called and asked about symptoms. If they exhibit symptoms, they are tested and are supposed to be given follow-up care. Month-by-month you count the number of disease-related events in the two groups and statistically test the difference.
No vaccine has completed a phase-3 trial so far—what other vaccine developers have published are preliminary, interim results. And the Oxford-AstraZeneca, NIH-Moderna and Pfizer-BioNTech vaccines were all authorized for emergency use before formally publishing interim phase-3 trial results. I am not too alarmed about the delay in Covaxin’s interim efficacy results, although I do consider that it is important as good practice and due process.
To my mind, a bigger failure lies in not having started other systematic trials, for example, a Covishield-Covaxin crossover trial, a study to test efficacy and safety of 1st dose Covishied, 2nd dose Covaxin and vice versa. If the government had started acting on this from January, when it approved both vaccines, by now, we would have got results too. [On 1 June, the government announced such trials.]
The inadvertent mixing of vaccines, as in the case of Siddharthnagar, is not too common right now, only because Bharat Biotech is still not producing more than 10% doses administered in this country. As Covaxin’s production scales up, this will happen more and more.
The concern with the absence of interim phase-3 results gets amplified because the Drugs Controller General of India (DCGI) has denied the data it reviewed to clear the vaccine. Given the financial windfall, people worry about the temptation to suppress adverse information.
Having inherited the colonial mindset, all governments in India are reluctant to disclose information. The DCGI is probably terrified of some incompetence being caught. And the consequence of this opacity is a disastrous loss of public trust.
With that said, I would be much more concerned about potential adverse effects if this were a drug. Vaccines do not by and large cause off-target adverse effects - these are more common with drugs. Vaccines do have rare allergic effects, as we have seen with Covishield too.
Finally, what advice might you offer the government?
Covid-related deaths and misery are a consequence of our general approach that the pandemic is a short term crisis, which will go away in a few months. Our response was episodic, as if each outbreak was like an earthquake that will pass, and then we can recover and go back to normalcy. This is why we did not have critical care support systems in a decentralized manner developed for an enduring period of time.
What we should have been systematically doing from last year, needs to be done this year. We need to invest more money. We need a much more proactive, systematic effort on enabling public sector production of Covaxin and diversifying vaccines platforms. Three months ago, we turned our noses up at Pfizer—we have now told them we will approve them.
We also desperately need a far better surveillance system, faster and comprehensive virus genome sequencing system, far better pre-clinical studies system where existing vaccines are tested for efficacy against new variants, and a systematic pipeline for next-generation vaccines. If we do that, then for Covid-19, we will have a 21st century system analogous to the 20th century influenza monitoring, surveillance and vaccine design system.
But for that we have to first acknowledge our limitations and failures. The political leadership of this government believes there cannot be any problem, because we cannot do anything wrong. Therefore, potential problems, roadblocks don’t need to be planned for. It’s triumphalist hubris that has brought us to this point.
(Aniket Aga is Associate Professor of Environmental Studies at Ashoka University.)