Updated: Aug 14, 2020
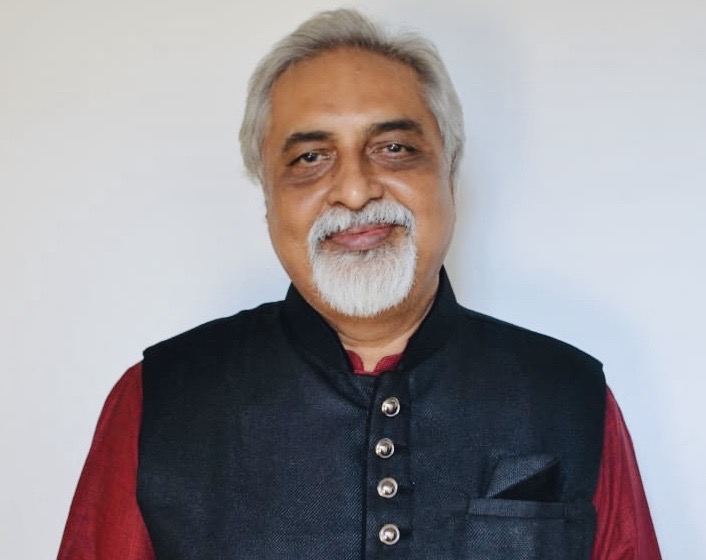
Mumbai: All his life, Dilip Purohit did everything he could to address governance failures in India’s richest city.
Alongside his day job as an administrative clerk at a small Mumbai garment factory, Purohit, 59, did what he could to improve his beloved city.
Some days, he would take issue with the city’s tardy public transport systems—dangerously overcrowded buses, trains delayed without explanation, auto-rickshaws refusing to ferry passengers. Other days, he would fight the opaque billing systems of telecom companies. He wrote complaints to public authorities, quoting to errant service providers their own rules.
Purohit believed in fighting the everyday battles of an average Mumbaikar. Some days, he lost. Some days, he won. The biggest of his battles was the last.
On 3 June 2020, as a cyclone called Nisarga slammed Mumbai, Purohit, infected with the coronavirus that causes Covid-19, died gasping for breath on his way to a hospital, after being denied admission over four hours.
Purohit was my uncle.
On that evening of 3 June, his fate illustrated the broken healthcare system in a city he loved, a metropolis of about 22 million, possessed with India’s best healthcare system.
Purohit’s story is also a warning to a country with more than 2 million reported cases—likely an underestimate—of Covid19, poised to spread into its vast, rural lands with scanty healthcare, according to experts (here and here). If that happens, India—with the world’s fastest Covid-19 growth rate since the first week of August—may vault into the world’s top spot by reported cases, from its current third position.
Mumbai, India’s Covid-19 Hotspot
Mumbai has held on to its status as India’s coronavirus hotspot over the last three months as the outbreak began in March and the virus spread nationwide.
As on 11 August, the city had 125,239 cases, more than 5.50% of India’s caseload of 2,268,675 cases. But Mumbai has a disproportionate share in Covid-19 deaths nationally, with 6,890 of 45,257, more than any other city and state in India. Delhi is a distant second with 4,131 deaths.
Mumbai’s death rate for coronavirus infections is 6% for detected coronavirus cases, three times the national average. It now has nearly 19,000 active detected infections, almost double the number of active cases in Delhi.
On 11 August, at least 1,100 patients were in critical condition, according to municipal data. Mumbai’s positivity rate,—the percentage of Covid-19 positive cases to the tests conducted—is around 20%, against the national average of 13%, a sign, experts told Article14, that the city needs to expand testing.
These data are backed by the findings of a recent sero-surveillance survey conducted by the Brihanmumbai Municipal Corporation (BMC), the Niti Aayog, Duke University in the US and others. A sero-surveillance survey detects the presence of antibodies—proteins the body produces when it detects foreign substances, such as viruses. Two in every five Mumbai residents were infected with the coronavirus and had developed antibodies, according to findings released on 28 July. In the city’s slums, the proportion was higher, with 57% exposed to the virus.
A comparison with similar surveys in other Indian cities indicates a greater spread of the coronavirus. In Delhi, a similar survey by the Indian Council of Medical Research (ICMR) revealed 22% of the population with antibodies; in Ahmedabad, 17.61% had been exposed.
Behind these data lie Mumbai’s dire healthcare realities: many patients, such as my uncle, denied beds; public hospitals overflowing with patients; private hospitals, scared of being shut down by city’s authorities, refusing to admit patients; and a refusal to test many with symptoms and desperate to be tested.
Social-media timelines revealed patients, family members and even doctors, angry and horrified in equal measure. Videos chronicled the collapse of healthcare. Some videos showed bodies piled up next to patients in crowded public hospitals, others overflowing hospital wards with infected patients lying in corridors, as they awaited treatment.
This three-part series (you can read part two and three here) chronicles the story of how Mumbai became, and remains, the country’s worst-hit Covid-19 hotspot. Pieced together through dozens of interviews with patients, families of Covid victims, government insiders and public-health experts, we discuss how Mumbai’s Covid-19 response led to a near-collapse of its municipal health infrastructure. Tens of people continue to die every day, three months after the outbreak started in early March.
Mumbai conducts fewer tests than Delhi, the country’s other major Covid hotspot. As of 11 August, Delhi with a population of about 20 million had conducted 1.2 million tests, compared to Mumbai’s 613,745 tests, according to BMC data. Over 20% of all samples in Mumbai tested positive. The World Health Organization (WHO) said on 12 May that the epidemic could be considered under control only when the rate was below 5%.
BMC chief I S Chahal, however, argued that Delhi’s testing numbers had been pushed up by including rapid antigen tests, which detect the presence of active virus proteins in less than 30 minutes. The accuracy of these tests can, often, be suspect, ranging, according to the WHO, between 34 to 80%.
“In Mumbai, an overwhelming majority of the tests we have conducted are RT-PCR tests, whereas Delhi has conducted a far smaller number of RT-PCR tests,” Chahal said, referring to the Reverse Transcription-Polymerase Chain Reaction (RT-PCR) test, which can take a few hours but is between 60 to 100% accurate.
He pointed to the BMC’s steps to push for more testing—on 23 June, Chahal announced Mission Universal Testing. “But even then, when testing did not pick up, we scrapped the need for a doctor’s prescription altogether on July 7. Anyone could now get tested,” Chahal told Article14, saying the BMC now has “zero restrictions” on testing.
Part one of this series discusses the systemic denial of testing and the failure of contact tracing. The second part chronicles how patients could not get hospital beds, worsened by official inability to mobilise private healthcare during the pandemic. The concluding part records the struggle of those seeking non-Covid healthcare for other serious, life-threatening ailments.
With the number of cases in the city refusing to ebb, Mumbai will also have to brace for its annual deluge of monsoon-related ailments, such as malaria and dengue. Mumbai’s failure to handle the pandemic has lessons for other cities now experiencing a surge in coronavirus infections.
A City Forewarned
Every year nearly 14 million travellers from 47 international destinations stream through Mumbai’s Chhatrapati Shivaji Maharaj International airport.
“Mumbai, being the country’s second busiest airport, was surely likely to be affected by the virus,” said Amar Jesani PhD, a city-based senior public health researcher and the editor of the Indian Journal of Medical Ethics. “It was clear that the virus was going to come from outside and infect people in Mumbai.”
The central government was slow to restrict the spread of the virus. On 17 January, over two weeks after the first cluster of cases emerged in China’s Wuhan city, it ordered three airports—Mumbai, Delhi and Kolkata—to start screening incoming passengers, but only those from China. Four days later, screening was extended to Chennai, Bengaluru, Hyderabad and Cochin airports, but remained focused on travellers from China.
Despite the WHO declaring a “Public Health Emergency of International Concern” on 30 January, it was only more than a month later on 4 March that the government of Prime Minister Narendra Modi announced that all incoming passengers would be screened.
The screening, as Mumbai soon realised, was barely a defence against the virus. It was perfunctory: thermal scanners recorded temperatures, and passengers within the normal range were released with no follow ups.
The government advised compulsory quarantine for travellers starting on 10 March, but for a handful of countries, such as China, Korea, Japan, Italy, Germany, Spain. It left out the Middle-East, a popular tourist destination and a busy transit hub for international travellers.
Mumbai would pay the price for this.
On 5 March, a day after the central government’s announcement for screening all passengers, a 63-year-old man landed in the city’s airport from Dubai after a business trip and decided to go straight home.
Two days later, he started feeling breathless and was admitted to a private hospital. Media reports said he had not revealed his travel history to doctors. Ten days later, he died and became India’s third and Maharashtra’s first coronavirus-related death.
By 15 March, Maharashtra had 33 cases, 18 of them people returning from Dubai, media reports suggested. Alarmed, the Maharashtra government, refusing to wait for the Centre to expand screening measures, announced on 16 March that it would compulsorily quarantine passengers coming in from the UAE, the US and Saudi Arabia. A day later, the Centre finally agreed to quarantine passengers from the UAE.
“We screened incoming passengers according to the list of countries that the Centre had given us,” said Chief Minister Uddhav Thackeray, while addressing the state on 11 April. “But, there were countries which were not included in the list, so they slipped through the screening and went into the community.”
The corporation had been pushing for an early ban on international flights, said Amey Ghole, a city corporator and chairman of the BMC’s public health committee: “We were screening for symptoms, but there were so many who passed through because they were asymptomatic,” he said.
Unclear Testing Protocols
Experts knew that Mumbai’s peculiar demographics meant a contagious virus would be hard to stop.
On average, 31,700 people live in 1 sq km of land in Mumbai, according to United Nations data. But over 40% of the population lives in teeming slums, which occupy only 8% of the city’s land. Population density in some slums can exceed 300,000 people per 1 sq km—10 times the city’s average.
When the virus came, it spread like wildfire. From 15 cases on 15 March, cases spiralled to nearly 1,900 over the next 30 days.
A crucial reason for this upswing was the lack of a clear testing protocol for those with Covid-19 symptoms and a refusal by the ICMR and, consequently, by the BMC, to test anyone except international travellers, as the BMC admitted.
Many who could have already been exposed to the virus were likely turned away.
When the first few cases in Mumbai were identified in places close to her workplace in Andheri West, 24-year-old Simran Singh* was worried that as an asthma patient, she was at risk. The fear turned real when she started experiencing breathlessness, coughing and fever on 10 March.
A day later, her brother, Rohit* experienced the same symptoms.
The siblings took a commuter train from their home in Bhayander, a far suburb, to the Kasturba Gandhi Hospital about 40 km away and the sole testing centre until then, a journey of more than 90 minutes—only to be denied tests.
“They said we had no travel history and there was no community transmission in Mumbai,” said Rohit. For the next 10 days, their symptoms got stronger and they remained bed-ridden. “My sister’s asthma flared up so much, she had to be rushed to a local hospital in Bhayander thrice,” said Rohit.
With Mumbai’s commuter trains shut down, mobility was restricted from 22 March; the two decided against going back to the Kasturba Gandhi hospital and instead quarantined themselves for 10 days.
It was not just in March, when testing kits were widely believed to be in short supply that tests were denied. Systematic denial of tests continued to be the hallmark of the BMC’s Covid-19 response until 7 July, when it announced that doctor prescriptions would no longer be needed for a Covid-19 test.
I witnessed this dissonance at close quarters.
The GuideLines That Led To Death
In late May, when my uncle started coughing, he decided to follow the BMC’s protocol by visiting a ‘Fever Clinic,’ temporary clinics that the BMC had set up in early April to test those showing symptoms of the virus.
The idea, as Chief Minister Uddhav Thackeray explained in a speech on 8 April, was that “anyone with fever, cold and cough should go to these clinics so that it can help us detect patients and prevent the spread”.
But Purohit was told that he was fine and did not need a test.
He returned, troubled. His cough was accompanied now by breathlessness.
Scared that he may have contracted the virus, he and his wife, Kokila decided to go to the BMC-run Rajawadi hospital in northeastern Mumbai, 10 minutes from their home, on 31 May. The queue was so long that Purohit, feeling breathless and weak, could not wait.
Back home, the family started calling private laboratories. But each lab insisted it needed a letter from a doctor prescribing the test. The family reached out to doctors it knew. Not one agreed.
Much of this reluctance was the BMC’s doing.
Through the last four months, the BMC has consistently tweaked its testing protocols that determine who is eligible for a Covid-19 test. By the middle of June, it had made tweaks eight times.
On 13 May, the BMC had said that symptomatic patients would be tested only if they had a doctor’s prescription. BMC commissioner Chahal told Article 14 that the civic body was only implementing 9 April ICMR guidelines, which allowed the testing of only symptomatic patients.
But between issuing the protocol and Purohit falling ill, the BMC started issuing “show-cause notices” to private doctors who had referred patients for tests without physically examining them. Just days before Purohit began to feel breathless, at least 20 private doctors had received BMC notices asking them to explain why their licenses should not be revoked, for “violating ICMR guidelines”, the Indian Express reported on 25 May.
After spending a day on the phone, trying to convince private labs to collect a sample, Purohit was finally taken to a private hospital, 40 minutes from home. Breathless, he was administered oxygen at the hospital because his oxygen saturation levels were low. Test done, he was sent home. On 2 June, he was told, the results would take 48 hours.
On 3 June, as Purohit’s breathlessness worsened, he could not find a hospital bed for over four hours. He died in his car on his way to a municipal hospital.
His test report, which arrived 24 hours after his death, revealed he had tested positive for Covid-19.
The Common Struggle To Get Tested
My uncle’s struggle with getting tested was a common one, I learned, after talking to tens of other Covid-19 patients in the city.
Pratik Shah*, 28, a resident of Juhu, told me he had such a tough time getting his 77-year-old grandmother, Meena Shah a test that doctors advised him to instead get a high-resolution computed tomography (HRCT) scan, a form of a CT scan, of her lungs.
Meena Shah had a dry cough for two days before she started having fever on 31 May. Since the septuagenarian was diabetic, Pratik Shah wanted to get her tested immediately.
But for two days the family struggled to get her tested.
“When we called private labs, they asked me for not just a doctor’s prescription but a letter from the BMC as well,” said Pratik Shah. He tried reaching the BMC. “One number was out of service. The other number told me I would need to go to the BMC office and check but the attendant did not know the procedure,” he said.
After two days, the desperate family got a HRCT scan. “The scan showed that she, most likely, had Covid,” said Pratik Shah. Meena Shah was finally admitted to a private nursing home close to home. But the delay took its toll. On 4 June, she died within 24 hours of being admitted.
‘Suppressing Numbers’
Such systemic obstacles in allowing patients to get tested are reflected in the BMC’s testing figures.
Starting with just over 1,100 tests every day on 1 April, BMC data show that the highest that Mumbai has been able to increase testing to was 11, 643 tests on 28 July. In the interim, its cases went from 169 on 1 April to over 111,964 on 30 July. So, while cases increased 66,150% between April and July, testing increased by 958% over the same period.
The BMC needs to expand testing, said Manoj Mohanan, an associate professor of public policy at Duke University in the US and part of the team that conducted the sero-surveillance study in Mumbai.
“The BMC still continues to mostly test mainly among symptomatic people and their contacts. In India, 95% of cases are asymptomatic (and they) are not being tested. Even among the symptomatic, many are scared of showing up for tests,” said Mohanan, pointing to Mumbai’s rate of more than 20% of all tests being coronavirus positive. “You are currently only testing those who approach the doctor themselves. If you do this, your positivity rate will continue to remain high.”
The refusal to expand testing also meant that, often, relatives of Covid-19 patients had to go to great lengths to be tested.
A BMC Congress corporator from Bandra, Asif Zakaria, said that he frequently receives SOS calls from relatives wanting to get tested.
“They first struggled to get a bed for their Covid-infected family members, and once that was done, they were made to run from pillar to post, to get their own tests done,” Zakaria said.
As a result many like 43-year-old Rashee Mehra* decide to pray instead.
Mehra’s 67-year-old father was detected with Covid on 10 June. But rather than being worried for her father she almost immediately turned her attention to her mother.
“My mother is a cancer survivor, has chronic asthma and suffers from diabetes and blood pressure, so I was very worried for her health,” Mehra said. For at least four days, her father had shown symptoms before he got medical care. In that time, her mother was constantly around him.
Even as they were getting her father admitted to a private hospital in central Mumbai, Mehra started looking out for ways to get her mother tested. She called private laboratories but they all asked for the same thing—a letter from the BMC.
A week earlier, on 3 June, BMC chief Chahal had issued fresh tweaks to the BMC’s testing protocols, allowing high-risk and direct contacts of Covid patients like Mehra’s mother to be tested without a doctor’s prescription. However, said Mehra, no laboratory was ready to do that.
For almost a week, Mehra worked the phone lines. She even tried to get in touch with local BMC officials to issue such a letter. But, the helplines of the local wards that the BMC had publicised, would either not be answered or when they were, officials failed to offer much clarity.
The Failure Of Contact Tracing
There was another common strand of municipal negligence connecting stories like my own with Mehra and Bhat: the absence of a municipal effort to track the source of the infection and, possibly, the spread of it from respective infected relatives.
WHO has listed contact tracing as “an essential public health tool” to help countries break the chains of transmission.
When Chahal took over on 10 May as the BMC chief, after the state government transferred the incumbent, Praveen Pardeshi, supposedly over his failure to control the spread of infection, he made contact tracing his priority. Chahal told his officers to increase the number of contacts traced for each positive case from the then-average of three to at least six.
Chahal said that the BMC had quarantined at least 15 contacts for every person detected to be Covid infected. “Since May, we focussed on the city’s slums and have quarantined 135,000 people who came in contact with an infected person in these slums,” he said. “This prevented the spread of the disease.”
However, none of the over dozen Covid patients and their families interviewed for this series said that the BMC had traced their contacts. This, public health experts said, points to the possibility of silent, asymptomatic spreaders in the community.
This negligence proved fatal to my family.
For three days after my uncle’s death no one from the BMC knocked on my family’s doors. His 57-year-old wife, Kokila, a diabetic, had fever while his daughter, 26, Aditi, experienced a loss of smell and a dry cough. Purohit’s mother, 87, was ailing and had started showing signs of breathlessness.
In what seemed like déjà vu, the family began calling various labs for tests. The labs wanted a letter from the BMC. The BMC did not respond to calls or texts to its local officials.
Kokila and Aditi even went to Mumbai’s municipal Rajawadi hospital, where they were told that the hospital was not conducting tests any more. They called the Kasturba Gandhi hospital, a municipal facility, the first to offer Covid19 tests, but were told the hospital did not conduct tests. The BMC helpline, 1916, promised a call back. It never came.
Aditi and her cousin Yash, who stayed in the same house, were rushed to a private hospital for a Covid test, where they both tested positive.
Three days later, Purohit’s 87-year-old mother, my grand-aunt, died without being tested.
This reportage was supported by the Thakur Family Foundation. The Thakur Family Foundation has not exercised any editorial control over the contents of this reportage
(Kunal Purohit is an independent journalist based in Mumbai.)
Part Two: Fear, Panic And Mumbai’s Missing Hospital Beds
Part Three: Meraj Shaikh’s Lost Body & Mumbai’s Non-Covid Victims